Insights / Articles
The patient as priority: How can effective internal training contribute to improving patient outcomes?
Written by Briony Frost on Thursday, October 8, 2020
Improving patient outcomes is a top priority for every healthcare professional (HCP). In a constantly evolving industry where knowledge, skills, techniques and technologies are frequently updated, continuous internal training for medical affairs professionals is an essential component of supporting positive patient outcomes. The “only way to provide safe, effective and high-quality healthcare” is for all health professionals to “maintain and improve their knowledge and skills throughout their careers.”[1]
Investing in ongoing education for med affairs staff brings obvious benefits. Effective training enables staff to:
- Improve their knowledge of disease totality and the clinical landscape
- Analyse and interpret clinical trial data
- Understand the products, devices and lifestyle management strategies available
- Communicate clearly and succinctly in a variety of ways with other HCPs
But how can we identify effective training for our teams and how can we be sure that it prioritises positive patient outcomes? The answer is to connect the dots between patient outcomes and med affairs teams’ professional practices within and throughout essential internal training programmes too.
This post is the first of a four-part blog series in which OPEN Health explains what these dots are and how they should be connected to maximise your team’s potential to positively impact patient outcomes. We start by exploring how to identify training programme approaches that will help your med affairs professionals support HCPs to make the right choices with their patients.
Identifying effective internal training
Many training providers specialise in either knowledge or skills development programmes. For example, Company X provides training on analysing complex data; separately, Company Y provides training on presentation skills. No matter how good the training provided by Companies X and Y, when knowledge development is divorced from skills development, a learning gap is created, in this case: how does the learner identify the key messages and present them to a healthcare audience, such as internal colleagues, medical practitioners, organisations, regulators and decision- and policy-makers, as well as patient groups.
If learners are left to extrapolate from Company Y’s skills training and adapt it to deliver the knowledge enhancement acquired from Company X, the results will vary depending on expertise, experience, confidence and prior training in each area, as well as how much was learned and retained from the original training programmes. This divergence in professional competencies – how skills are used to apply scientific content knowledge to the real world – may impact the information received by the audience. Impacts here include the loss of valuable knowledge gains, inefficient system usage, frustrated users, dissatisfied patients and potentially poor outcomes, wasted time, reputational damage and reduced financial performance – in addition to the initial money and time put into creating and delivering two separate training programmes.
Instead of training content and skills separately, look for programmes that:
- Engage with learners, as well as the leadership team, ahead of delivery to identify and benchmark specific skills and knowledge gaps within the context of their roles
- Enable learners to develop core content knowledge and relevant skills simultaneously, such as distilling, prioritising and presenting key data succinctly and clearly to appropriate audiences
- Integrate applied learning scenarios, such as case studies, problem-solving activities, simulations, virtual realities and role-play to enable learners to practice making use of their knowledge through their skills
- Provide robust, real-time feedback on practice activities and assessments
- Incorporate robust programme evaluation and training impact measures
- Create materials that have been designed and approved for repurposing, adapting and delivering to other HCPs
Improving patient outcomes
Training that encompasses the above is likely to be more effective (both in terms of cost and learning gain) as well as more efficient. But how can we be sure? We will explore the metrics aspect of this question in more detail in the third instalment of this blog series, but before we can look at the results of evaluations, we have to be sure that the training is designed to meet achievable and measurable outcomes.
While training providers are increasingly shifting towards instructional design methods, it is still fairly commonplace for internal training to be designed to fit around perceived essential scientific content knowledge, not what the learner needs to be able to do with that knowledge after the training is complete. This is not an ideal scenario. What happens, consciously or unconsciously, is that a “content-centred” curriculum is developed[2]:
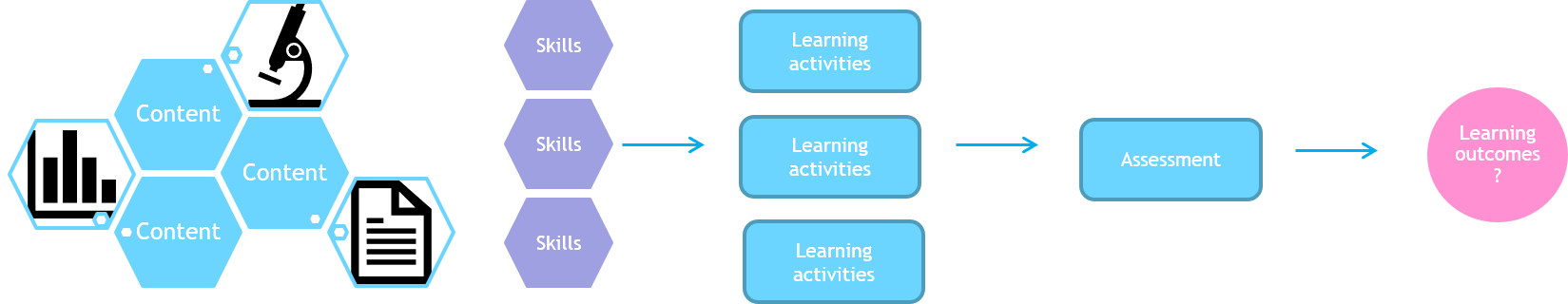
Figure 1: Adapted from G. Wiggins and J. McTighe, Understanding by Design 2005. Accessed 30/09/2020.
Here, content is king: learning activities are built around it, skills are delivered separately or bolted on later, assessments are constructed as an afterthought and what successful outcomes look like is often unclear.
Instead, look for training that is designed with what learners need to be able to do to support positive patient outcomes first. Providers should:
- Analyse your team’s learning needs from the outset
- Identify intended learning outcomes from the outset and map them against learner and company key performance indicators (KPIs)
- Understand and explain how learning outcomes, assessments, learning activities, and content plus skills are connected, and why they should be designed in that order
- Distinguish between need to know, useful to know and nice to know content
- Explain how achievement against the learning outcomes will be measured and evaluated to demonstrate impact on professional performance and, by extension, patient outcomes
Thinking along these lines produces a “learning-centred” curriculum[3]:
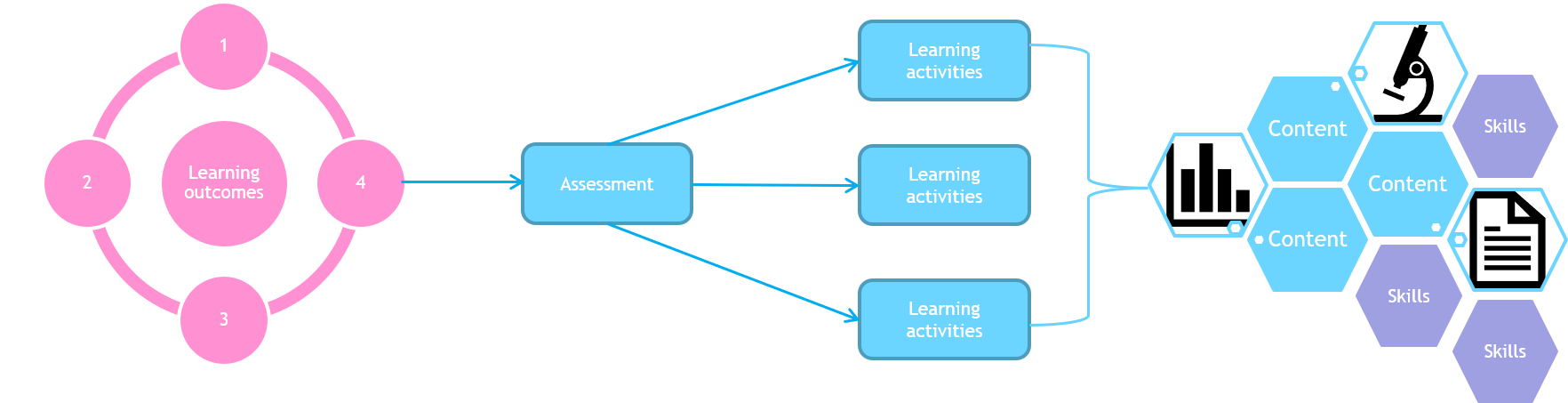
Figure 2: Adapted from G. Wiggins and J. McTighe, Understanding by Design 2005. Available at: http://www.ascd.org/research-a-topic/understanding-by-design-resources.aspx. Accessed 30/09/2020.
Here, desired results are identified first, followed by a determination of acceptable evidence and finally the planning of learning experiences, instructions and resources required to enable learners to provide evidence that they have met the learning outcomes.[4] Using this model, priorities are easier to determine; learning outcomes, assessments and activities are integrated more effectively; and clarity and consistency support a more accurate construction of course concepts, providing concrete, achievable, measurable outcomes.
A number of other factors, such as the metrics that are used and how learner motivation, engagement, confidence and mental health are supported (which we will discuss in our next instalment), are critical to maximising the success of any training programme. But connecting the dots between patient outcomes and each internal training programme’s intended learning outcomes, and keeping the core aspects of the training programme joined up too, is a great place to start!
[1]“The Importance of Continuous Education in Healthcare,” Health Management 2017;17(2). Available at: https://healthmanagement.org/c/healthmanagement/issuearticle/the-importance-of-continuous-education-in-healthcare. Accessed 30/9/2020.
[2]L.D. Fink, Integrated Course Design 2013. Available at: https://www.ideaedu.org/Portals/0/Uploads/Documents/IDEA%20Papers/IDEA%20Papers/Idea_Paper_42.pdf. Accessed 30/9/2020.
[3]D. Fink, 2013.
[4]G. Wiggins and J. McTighe, Understanding by Design 2005. Available at: http://www.ascd.org/research-a-topic/understanding-by-design-resources.aspx. Accessed 30/09/2020.
For information about OPEN Health’s services and how we could support you, please get in touch.